 Click to Print Adobe PDF
Click to Print Adobe PDF
Fall 2009 - Vol.4, No.3
Hazards of Ingested Magnets
Attila G. Devenyi, M.D.
Regional Gastroenterology Associates of Lancaster, Ltd.
|
 |
INTRODUCTION
Ingestion of a foreign body, whether inadvertent or intentional, is a common clinical problem. The American Association of Poison Control Centers reported over 100,000 incidents of ingestion of foreign bodies by children and adolescents in the year 2000.[1] The vast majority of ingestions are accidental, with the peak incidence in children occurring between six months and three years of age. Intentional ingestions occur with increasing frequency in the adolescent years. In the United States, the most commonly ingested foreign bodies are coins, followed by myriad other objects including toys, toy parts, jewelry, batteries, and a wide variety of small objects such as house keys and dental appliances. Even a toothbrush has been accidentally ingested by a bulimic patient.
The majority of ingested objects pass through the alimentary tract without complications. Intervention is required in certain circumstances, however, such as when a coin lodges in the esophagus, or an object that contains potentially toxic material such as lead or a battery. Occasionally, an esophageal foreign body is identified on a chest x-ray in a child who is undergoing evaluation of wheezing or other respiratory problem.
As discussed further below, however, ingested magnets pose unique challenges. Building sets and toys are commonly manufactured for children with powerful rare earth magnets (commonly neodymium iron boron or samarium cobalt magnets). Their small size increases their potential for ingestion by children who commonly put objects in their mouths. In many toys the magnets are embedded in plastic parts and can be easily detached. In Asian countries magnetic beads and necklaces are worn for their purported healing power. In the United States, the use of magnets is frequently described in the literature on complementary and alternative medicine.
THE HAZARDS OF INGESTED MAGNETS
The following case is presented to alert the reader to the unique risks inherent in this apparently benign occurrence, and to outline an approach that emphasizes early and aggressive intervention to prevent significant morbidity and possibly mortality.
Case Report
A 7-year-old child was brought to the emergency room by his grandmother with a chief complaint of abdominal pain. The pain was of sudden onset, and occurred while the child was playing a computer game. When asked where the pain was most severe, the child pointed to the upper abdomen. There was no vomiting or diarrhea. There was no history of fever and the child had recently consumed a normal lunch. The child's past medical history included ADHD, for which he was taking Concerta, 18 mg once daily. There was no other significant past medical or surgical history. Examination showed an alert and oriented child. Blood pressure was 104/51, pulse 60, respirations 20. He was afebrile. He rated his pain at 7 on a scale of zero to 10. He was not dysmorphic. HEENT exam was unremarkable. Neck was without adenopathy or thyromegaly. Chest exam showed clear and equal breath sounds. Cardiac exam revealed regular rate and rhythm with normal S1 and S2. Abdominal exam revealed focal reproducible tenderness in the epigastric region. There was no lower abdominal tenderness, organomegaly, or masses. Bowel sounds were normal.
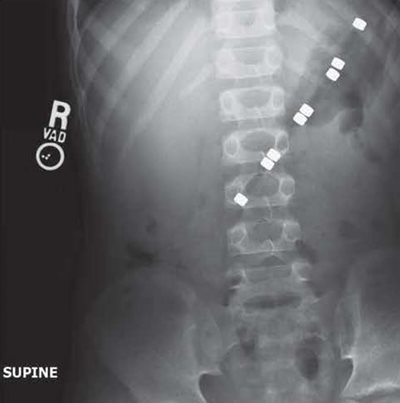
Figure 1
An obstructive abdominal x-ray series was obtained (left). The interpretation read: "Supine and upright views of the abdomen show an elongated rod shaped radiopaque structure measuring maximally 12 cm. in length and about a centimeter in width which lies obliquely within the stomach. It has 8 dense radiopaque elements. The bowel gas pattern is normal. The osseous structures are intact."

Figure 2
After additional questioning the child admitted to swallowing multiple magnets the evening before in a fit of anger. (Figure 2) The ingestion was witnessed by his uncle, but not reported to other family members.Endoscopy was then performed emergently under general anesthesia to retrieve the foreign bodies. A single magnet was visualized along the lesser curve of the posterior aspect of the stomach. An additional magnet was visualized in the second part of the duodenum (Figure 3). The gastric foreign body was then removed using a Roth Net foreign body retriever. The endoscope was then reinserted and the magnet in the duodenum was netted and removed. The endoscope was inserted a third time simultaneously removing the last two magnets which remained attached to each other during retrieval. There were no complications during the procedures. Inspection showed superficial erosions in the gastric mucosa at the site where the magnet had been removed. The corresponding distal duodenal site could not be visualized. The child was observed overnight. In the morning he was pain-free, tolerated a regular diet, and was discharged in good health.

Figure 3
Background
The majority of ingested foreign bodies traverse the gastrointestinal system spontaneously without complication. Their management depends upon the nature of the ingested object and its location in the gastrointestinal tract, as well as the age and past history of the patient. Esophageal foreign bodies should be urgently removed because of their potential to cause significant morbidity. Batteries lodged in the esophagus, sharp objects in the esophagus or upper gastrointestinal tract, and objects comprised of toxic material such as lead all require urgent endoscopic removal. Small, blunt objects below the diaphragm can generally be managed conservatively by inspection of the stool and radiographic surveillance.[2]
A single small magnet, like any other foreign body, will most likely pass through the gastrointestinal tract without complications. On the other hand, multiple magnets, or a combination of magnets and metallic objects, pose a unique hazard due to their propensity to attract each other while residing in different loops of bowel.
s ingested magnets proceed through adjacent loops of bowel, they attract each other and compress the intervening bowel wall. This compression ultimately leads to pressure necrosis which results in perforation, fistulas, and even volvulus, with significant morbidity and rarely mortality.[3]
A case reported by Cauchi and Shawis illustrates this process.[4] A 9-year old girl ingested 12 small magnets on separate occasions a week before presenting with abdominal pain, vomiting, and diarrhea. At laparotomy she was found to have multiple ileal perforations and the 12 magnets which had adhered to one another were lying free in the peritoneal cavity. Similar findings have been reported with the ingestion of a magnet and other metallic objects by Nagaraj and Sunil.[5] In another case the parents of an otherwise healthy 4-year-old boy witnessed him swallowing a small magnetic piece from a toy set.[3] The following day his parents witnessed him swallow a second identical magnet. His parents assumed the magnets would pass in the stool, however, after 72 hours he developed left sided abdominal pain prompting an emergency department visit. Radiographs showed what appeared to be two magnets in the cecum. Surgery revealed a loop of terminal ileum adherent to the mid-right colon with omentum walling off the area. Removal of the omentum revealed an acute fistula in which the two magnets were situated. These cases illustrate how perforations and fistulas develop, but also suggest the need for some interval to pass between ingestions of the magnets. If ingested simultaneously, it is likely that they will attach in the stomach and pass simultaneously. In the case reported herein, the magnets were likely ingested within a fairly short interval, allowing the gastric magnet to "anchor" the others, which were likely ingested shortly before. Though fistula formation and perforation are the most common complications that occur beyond the upper gastrointestinal tract after ingestion of multiple magnets, volvulus has also been reported. An area of fixation by the magnets can act as point of volvulus, leading to bowel necrosis, sepsis, and death. Likewise, fixation of two loops of bowel can lead to obstruction.
A case series of 20 children that further illustrates the epidemiology and complications of magnet ingestion was published by the Centers for Disease Control in 2006.[6] The patients ranged in age from 10 months to 11½ years. Sixteen (80%) were >3 years of age. The majority (80%) were male. There was one fatality, a boy age 20 months, who died following midgut volvulus with necrosis and septicemia after ingesting magnets dislodged from an older sibling's toy. All other cases included severe complications such as bowel perforation (15), bowel obstruction and peritonitis (4 cases), and volvulus (3 cases). The report specifically noted that the initial signs and symptoms of injury can be mild and non-specific, leading to a delay in diagnosis and greater injury. The hospital length of stay ranged from 3 to 19 days; at least five patients required intensive care. The number of magnets swallowed ranged from one (plus a nonmagnetic metal piece) up to 15 magnets. (Up to 32 magnets aligned in tandem in a cylindrical structure have been reported.[7] In 12 cases magnets had been dislodged from other toys, and in 3 circumstances entire magnetic pieces were swallowed intact. Five children swallowed the magnet or magnetic pieces intentionally.
Of the 20 cases, five children had potentially relevant conditions, including one with autism, two with ADHD, and two with other neurological disorders and developmental delay. Others have reported ingestion of magnets in children with neurodevelopmental disorders including absence of the corpus callosum with developmental delay[8] and Beckwith-Weidemann syndrome and significant developmental delay.[9] Anselmi and coworkers, in a case report and review, also noted a similarly high frequency of neurodevelopmental disorders in 4 of 14 patients.[10] The fact that the patient reported in the present paper was male, over 3 years of age, had ADHD, and intentionally ingested the magnets, is consistent with this historical pattern.
MANAGEMENT
When ingestion of a foreign body is reported by a caretaker, it is important to ascertain whether or not the object may be magnetic. The presence of magnetic toys or other magnetic objects in the household, such as magnets used for relief of musculoskeletal complaints, should be ascertained. To aid in diagnosis, a compass may be passed over the abdomen6; deflection suggests the object is magnetic, though the absence of deflection does not rule it out. (This maneuver must be done in an area clear of magnetic fields such as those generated by computer monitors or electronic equipment.) If a provider suspects that a magnet has been ingested, an immediate radiographic evaluation is recommended. Delay may allow the ingested magnet to pass beyond the reach of the endoscope. If the magnet is thought to be located within the reach of the endoscope, emergency endoscopy is indicated to retrieve the objects before they pass distally.
The radiographic distinction between the ingestion of multiple magnets and a single magnet may be subtle or impossible to determine. Magnetic forces cause the alignment and close apposition of multiple units and can make multiple magnets appear as one. In one instance a misdiagnosis and misconception that a solitary magnet was ingested led to premature discharge from the hospital and the patient's subsequent return with an abdominal perforation resulting in an emergency laparotomy.[11] Additional radiographs or fluoroscopy may be useful to determine if the metallic foreign body is truly a single object or the close unification of multiple similar sized and shaped magnets. Subtle separation or gaps suggest the presence of bowel wall between the objects, though the absence of a gap does not exclude the possibility of multiple closely adherent magnets. The absence of movement on follow-up radiographs should also raise the suspicion of magnetic objects apposed across bowel wall.
The increase in case reports related to magnet ingestions and the severity of the accompanying complications has resulted in several papers calling for a separate treatment regimen for patients ingesting multiple magnets..[12].[13] If more than one magnet or a magnet and other metallic foreign bodies have been ingested and are beyond the reach of the endoscope the surgical service should immediately be consulted and inpatient observation initiated. Serial physical examinations and radiographs should be obtained to assure progression of the objects through the alimentary tract until they have passed. Surgical intervention should be undertaken at the first sign of obstruction or increasing abdominal pain. This algorithm may prevent the more serious complications reported in the literature. The insensitivity of plain radiography and computed tomography in determining the number of magnets has led Butterworth and Felis to suggest that any magnet ingestion should be treated as if multiple magnets were ingested..[11]
CONCLUSIONS
All physicians and healthcare providers involved with children should be aware of the problems caused by ingestion of magnets. Although reports of multiple magnet ingestions are rare, the literature illustrates that the magnetic attraction of foreign bodies located in different sections of the gastrointestinal tract can lead to serious complications such as perforation, obstruction, fistula, volvulus, and death. Given these findings, a patient suspected of magnet ingestion should be referred for immediate evaluation, including abdominal radiographs. If possible, the magnet should be removed by emergency endoscopy. If the magnets have passed beyond the reach of the endoscope, surgical consultation, inpatient observation with serial radiographs and abdominal examinations, should be performed. If the objects are stationary, or if signs of obstruction or increasing abdominal pain are present, then operative intervention should be performed to retrieve the objects to prevent further complications. Ingested magnets need to be treated differently from other ingested objects because of a higher associated morbidity.
References
[1] Litovitz TL, Klein-Schwartz W, White S et al. 2000 Annual report of the American Association of Poison Control Centers Toxic Exposure Surveillance System. Am J Emerg Med 2001; 19:337-395.
[2] Uyemura M. Foreign body ingestion in children. Am Fam Physician 2005;72(2):287-291
[3] Dutta S, Barzin A. Multiple magnet ingestion as a source of severe gastrointestinal complications requiring surgical intervention. Arch Pediatric Adolesc Med 2008;162(2):123-125.
[4] Cauchi JA, Shawis RN. Multiple magnet ingestion and gastrointestinal morbidity. Arch Dis Child 2002;87:539-540.
[5] Nagaraj HS, Sunil I. Multiple foreign body ingestion and ileal perforation. Pediatr Surg Int. 2005;21(9):718-720.
[6] Gastrointestinal injuries from magnet ingestion in children: United States, 2003-2006. Centers for Disease Control and Prevention (CDC). MMWR Morb Mortal Wkly Rep. 2006;55(48):1296-1300.
[7] Uchida K, Otake K, Iwata T et.al.. Ingestion of multiple magnets: hazardous foreign bodies for children. Pediatr Radiol 2006;36:263-264.
[8] Liu S, Blacam C, Lim F et.al.. Magnetic foreign body ingestions leading to duodenocolonic fistula. J Pediatr Gastroenterol Nutr 2005;41:670-672.
[9] Pryor HI, Lange PA, Bader A et al. Multiple magnetic foreign body ingestion: A surgical problem. J Am Coll Surg 2007;205(1):182-186.
[10] Anselmi EH, San Roman CG, Fontaba JEB et. Al.. Intestinal perforation caused by magnetic toys. J Pediatr Surg 2007;42:E13-E16.
[11] Butterworth J, Feltis B. Toy magnet ingestion in children: revising the algorithm. J Pediatr Surg 2007;42:E3-E4.
[12] Kay M, Wyllie R. Pediatric foreign bodies and their management. Curr Gastroenterol Rep 2005;7:212-218.
[13] Vijaysadan V, Perez M, Kuo D. Revisiting swallowed troubles: intestinal complications caused by two magnets. A case report, review and proposed revising of an algorithm for the management of foreign body ingestion. J AM Board Fam Med 2006;19:511-516.
Attila G. Devenyi, M.D.
Regional Gastroenterology Associates of Lancaster, Ltd.
2104 Harrisbug Pike, Suite 300
Lancaster, PA 17604
717-544-3400
agdeveny@LGHealth.org