
Winter 2016 - Vol. 11, No. 4
Effective Non-Opioid Treatment Options
for Low Back Pain
Tony T. Ton-That, M.D., FABPM&R
Medical Director, Spine and Low Back Pain Program
Lancaster General Health
INTRODUCTION
Low back pain is the leading cause of disability in the United States, accounting for nearly 15 million medical visits and $25 billion in health care spending annually. One major consequence of the condition, prescription opioid abuse, imposes an enormous societal burden. In 2007 it was noted that despite representing less than 5% of the world’s population, the United States consumes 99% of the world’s hydrocodone supply.
1 In 2012, there were 259 million prescriptions for painkillers in the U.S., or more than one prescription for each adult.
2
The prevalence of osteoarthritis (OA), low back pain (LBP), and musculoskeletal pain is increasing as a result of an aging population, the epidemic of obesity, sedentary jobs, and inactive lifestyles. Up to 84% of adults have low back pain at some time in their lives, and over one-quarter of U.S. adults report recent low back pain in the past three months. Treatment of acute and chronic musculoskeletal, non-cancer pain is complex and requires the use of multiple strategies and resources.
COMMON ETIOLOGIES OF LOW BACK PAIN
Nonmalignant spinal pain, especially LBP, is by far the most common cause of both acute and chronic pain encountered in daily medical practice. Acute LBP can be the result of muscle strain, ligamentous sprain, diskogenic pathology (annular tear, disk herniation), or sensory nerve root/spinal nerve injury. Acute low back pain also can emanate from inflammation of the facet, also known as the zygapophysial joint (such as synovitis, capsular stretch or tear), or a compression fracture of a vertebral body.
MANAGEMENT OF LOW BACK PAIN
Pharmacologic treatment is often effective in the short term, but long-term use of medications has limited benefit because of potentially dangerous side effects. Nonsteroidal anti-inflammatory drugs can damage the kidneys, GI tract, liver, or heart; antidepressants can cause hypotension, constipation, and other anticholinergic side effects; and antiepileptic medications can cause cognitive impairment, weight gain, and mood alterations.
Back pain can be treated successfully by early intervention and physical therapy, without the need for opioids or costly imaging tests, which have questionable value for most patients. In addition, medications comprise a passive treatment that does not empower the patient with the independence of self-management.
Physical therapy
Early referral to the care of a physical therapist has been shown to decrease the likelihood of acute LBP becoming a chronic condition.
3 An individualized therapy program for both acute and chronic pain conditions should be developed to address the problems. The affected musculoskeletal tissues will be evaluated by targeted physical examination to assess their tolerance to stress, such as direct pressure on injured tissue, loading of a reactive joint, or active ranging of an extremity. Any stress intolerances require intervention and a designated target for improvement after therapy.
Physical modalities
Therapeutic ultrasound is used to decrease muscle spasm and pain, and to facilitate extensibility of soft tissue and joints.
Transcutaneous electrical nerve stimulation (TENS) is the safe and noninvasive application of pulsed current to relieve pain through stimulating A Delta nerve fibers to inhibit pain transmission to the brain based on gate control theory.
Exercises can increase strength, and can restore flexibility, mobility, good balance coordination, and endurance. Passive exercise is completed externally from a physical therapist without any voluntary contraction of muscle by the patient. These exercises are most useful in the initial phase of improving flexibility and joint range of motion. Active exercise require muscular contraction from the patient. A home exercise program is a necessary part of the overall exercise regimen.
Movement-based physical therapies provide both education and exercise to complement manual therapies as part of a multimodal approach.
 Fig. 1. Flexion-biased exercises (when sitting feels good).
Fig. 1. Flexion-biased exercises (when sitting feels good).
Flexion-biased exercises (Fig. 1) are useful for posterior axial spinal pain that may be reduced or localized by flexing the spine. The goal is to open intervertebral foramina and facet joints. These exercises are used to decrease facet joint compressive forces and stretch the lumbar extensors, including the posterior ligamentous and myofascial tissues.
 Fig. 2. .Extension-biased exercises (when standing feels good).
Fig. 2. .Extension-biased exercises (when standing feels good).
Extension-biased exercise (Fig. 2) such as the McKenzie program may be useful with patients who have radicular pain due to disc herniation. These exercises facilitate centralization of pain away from the feet, legs and buttock while pain may simply persist at the back.
Mind and body exercises like Tai Chi, Yoga, and Pilates promote mental focus and attention alongside slow movements, which further address the psychologic aspects of pain.
Tai chi is a Chinese martial art based on slow, continuous movements coordinated with breathing to enable meditation with movement that seeks to balance internal energy, or “qi,” and mediate physical and psychological well-being.
Yoga includes physical exercise through specific movements and poses with mental focus through meditation and breathing to improve posture, flexibility, and strength, and to reduce stress and anxiety, thus providing pain relief.
Pilates emphasizes core strengthening, body alignment, improvement of posture and coordination, with controlled whole-body movements by the use of specific equipment, along with coordination of breathing and concentration, to promote both physical and mental health.
COMPLEMENTARY MEDICINE TECHNIQUES
Besides movement-based physical therapies and manual therapies, acupuncture is a complementary treatment for pain management.
Acupuncture is part of an ancient system of health care in China going back more than 500 years, and is based on the concept that energy (called Qi or Chi) flows through the body in certain patterns (meridians); the free flow of this energy ensures good health. Blockages of the free flow of energy in one of the meridians causes energy imbalances, and are believed to lead to symptoms such as pain, weakness and eventually disease. Acupuncture is thought to unblock these obstructions to allow free flow of energy and thus relieve symptoms.
Acupuncture is done by inserting sterile disposable thin needles at very precise acupuncture points that follow the energy channels (meridians). The needling at acupuncture points stimulates the release of central nervous system endorphins and chemicals that are known to be involved in mood and pain perception (serotonin, GABA, catecholamine, and dopamine), and influences one of the body’s pain generating messengers as substance P. Infrared heat and/or electrical stimulation can also be applied, to provide a synergistic effect with acupuncture needles. Evidence suggests that acupuncture is effective for short-term pain relief in neck and low back pain, lateral epicondylitis, rotator cuff tendonitis, fibromyalgia, and myofascial pain.
4 Acupuncture has also previously been discussed in this Journal regarding cancer therapy.
5
Acupressure is another complementary technique that has been effective in treating acute LBP; direct pressure is applied over trigger points to decrease myofascial pain.
Therapeutic massage applies rhythmic pressure and stretching to soft tissues using various techniques to relieve pain. Alternative therapies like
Rolfing incorporate deep-tissue manipulation and movement training to improve body alignment and biomechanics.
Cupping is a traditional Chinese medicine (TCM) therapy dating back at least 2,000 years. Types of cupping include retained cupping, flash cupping, moving cupping, wet cupping, medicinal cupping, and needling cupping. The actual cup can be made of materials such as bamboo, glass, or earthenware.
The mechanism of cupping therapy is not clear, but some researchers suggest that placement of cups on selected acupuncture or tender points on the skin produces hyperemia or hemostasis, which results in pain relief. Cupping treatment was used by some of the athletes at the 2016 Summer Olympic Games seeking pain relief and accelerated recovery from soft tissue and myofascial injury.
PERCUTANEOUS MANAGEMENT
Trigger point injections: Trigger points are discrete, focal, hyperirritable spots located in a taut band of skeletal muscle. They produce pain locally and in a referred pattern, and often accompany chronic musculoskeletal disorders. Acute trauma or repetitive micro trauma may lead to the development of stress on muscle fibers and the formation of trigger points. Palpation of the trigger point will elicit pain directly over the affected area and cause radiation of pain toward a zone of reference and a local twitch response.
Various modalities, such as the Spray and Stretch technique, ultrasonography guided injections, manipulative therapy and injection, are used to inactivate trigger points. Trigger-point injection has been shown to be one of the most effective treatment modalities to provide prompt relief of symptoms due to myofascial injury.
Piriformis syndrome is a common cause of buttock and posterior leg pain. The tight piriformis may cause a nerve entrapment syndrome as a consequence of its close proximity to the sciatic nerve. Piriformis injection can help to relieve the symptoms.
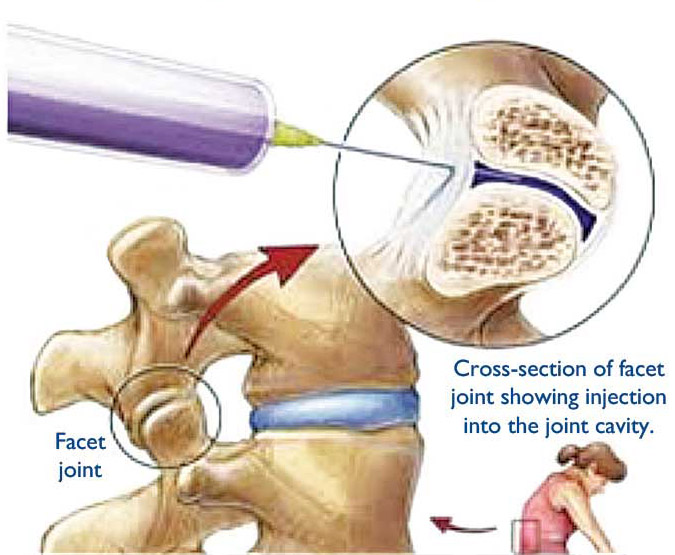 Fig. 3. Facet joint block injection.
Fig. 3. Facet joint block injection.
Facet joint injection (Fig. 3): The injection of local anesthetic and/or steroids into the facet joint is offered to patients in whom it is believed the facet joint is the cause of the symptoms of their back pain, but the effectiveness of this therapy for short- and long-term pain relief requires further evaluation. Facet joints have a capsule that is richly innervated by the medial branches of the posterior lumbar rami (branches of the lumbar spinal nerves).
A medial branch block is similar to facet joint injection but the medication (with or without steroids) is placed outside the joint space near the medial branches of the posterior lumbar rami. If medial branch block provides short-term relief,
radiofrequency ablation (RFA), a procedure that heats the spinal nerve to interrupt pain signals, is an emerging treatment option for long lasting effect for chronic axial back pain due to facet syndrome or sacroiliac joints.
Sacroiliac injection: The sacroiliac joint is a common source of low back pain as well as referred pain into the buttock, groin, and lower extremities. Degeneration of the sacroiliac joint can be caused by numerous conditions, including degenerative and inflammatory arthritis, trauma, ankylosing spondylitis, pregnancy, lumbosacral fusion, hip arthritis, limb length inequality, infections, and neoplasia.
Sacroiliac joint pathology has historically been difficult to diagnose solely on clinical signs and symptoms, and the gold standard for diagnosis is image intensifier–guided injection of a local anesthetic. (Fig. 4)
 Fig. 4. Sites of potential stenosis in the spinal canal.
Fig. 4. Sites of potential stenosis in the spinal canal.
Epidural steroid injection: For the treatment of radicular lumbar and lower extremity pain, caudal, interlaminar, and transforaminal epidural steroid injections have gained rapid and widespread acceptance. All techniques have limited benefit, however, in managing post laminectomy syndrome and spinal stenosis.
6 The potential advantages of transforaminal over interlaminar and caudal routes include targeted delivery of a steroid to the site of pathology, presumably onto the inflamed nerve root.
7
Spinal cord stimulation for chronic pain syndrome and failed back surgery syndrome: Neuromodulation with Spinal cord stimulation (SCS) is one of the developments in chronic pain management. It has been used for chronic neuropathic pains that have been refractory to other conventional treatments. The technique is believed to inhibit chronic pain by stimulating the large diameter afferent nerve fibers in the spinal cord, which is based on the gate control theory of pain proposed by Melzack and Wall.
8 (Fig. 5.)

Fig. 5. Spinal cord stimulation therapy uses mild electrical
impulses to help manage chronic pain. A small, external
remote device signals a pulse generator implanted in the
lower back to send low currents of electricity through
extension wires to leads in the spine. This creates a tingling
sensation that masks pain signals as they travel to the brain.
Photo courtesy of Boston Scientific.
Medication management
Nonsteroidal anti-inflammatory drugs (NSAIDs) are the most commonly used drugs for management of adults with low back pain. NSAIDs can decrease inflammation by blocking enzymes that produce prostaglandins, the naturally occurring fatty acids that play a role in pain and inflammation. Older NSAIDs like ibuprofen block both COX-1 and COX-2, but celecoxib (Celebrex®) targets mainly COX-2. It is important to remember that celecoxib is not more effective than other NSAIDs; its advantage is related to lower risk of gastric irritation and peptic ulcers because of its selective inhibition of Cox-2.
All NSAIDs have been associated with a risk of heart attacks and strokes, especially with chronic use. Celecoxib is considerably more expensive, though that problem has been greatly alleviated by the expiration of the patent on Celebrex®, and the availability of generic versions. It addition, celecoxib was thought to have a higher risk of myocardial infarction than non-selective NSAIDs, but a recent study appears to eliminate that concern.
9
Alternatively, acetaminophen can be used for acute low back pain relief.
Gabapentin (Neurontin®, Pfizer Pharmaceu-ticals) and pregabalin (Lyrica®, Pfizer Pharmaceuticals) are antiepileptic drugs that are approved by the FDA for treatment of post herpetic neuralgia and painful diabetic polyneuropathy, phantom limb pain and fibromyalgia. They are structurally similar to gamma-aminobutyric acid (GABA), although they do not bind to GABA receptors. They are thought to exert their beneficial effects on neuropathic pain by binding to the α-2-delta subunit of voltage-dependent calcium channels, which leads to reduction of calcium influx into neurons throughout the central nervous system and may in turn decrease the release of glutamate, norepinephrine, and substance P.
Alternatively, anti-depression medications of the serotonin, norepinephrine reuptake inhibitor class (SNRIs) can be effectively used for chronic low back pain.
Pain Neuropsychology
Predictors of chronicity are primarily related to psychosocial factors which include existing psychological comorbidities, maladaptive coping strategies (avoiding activities because of fears they will further damage the back), and catastrophizing (anticipating the worst possible outcomes from low back pain). Over the past three decades, cognitive-behavioral therapy (CBT) has become a first-line psychosocial treatment for individuals with chronic pain. Evidence for efficacy in improving pain and pain-related problems across a wide spectrum of chronic pain syndromes has come from multiple randomized controlled trials. Recently, the Cleveland Clinic demonstrated a successful pilot program that initiated psychology and physical therapy as the first line of treatment for chronic pain management.
CONCLUSIONS
Opioid medications are not the first line of treatment for acute low back pain due to ineffectiveness, side effects, and risks of dependency. There are numerous pharmacological, interventional, and complementary alternative evidenced-based treatments that can be offered to patients as the first line of treatment. Functional improvement and pain reduction will be achieved without using opioid medications. More research is needed to understand the selection of optimal treatments, and the combination and sequencing of treatments for low back pain.
Lancaster General Health has taken an innovative, triple aim-focused approach to treating low back pain. The new system-wide program has reduced opioid prescriptions for acute low back pain by more than 20% in the emergency department and by 10% in primary care offices. The Hospital and Health System Association of Pennsylvania’s Optimal Operation Award for 2016 was given to Lancaster General Health for the program,
Transforming Care for Low Back Pain: A New Population Health Model.
REFERENCES
1. Report of the International Narcotics Control Board for 2007. United Nations, New York, 2008.
http://www.incb.org/incb/en/publications/annual-reports/annual-report-2007.html.
2. Centers for Disease Control and Prevention. CDC Vital Signs: Opioid Painkiller Prescribing. July 2014. Atlanta, GA: Centers for Disease Control and Prevention; 2014.
3. Wand BM, Bird C, McAuley JH, et al. Early intervention for the management of acute low back pain: A single-blind randomized controlled trial of biopsychosocial education, manual therapy, and exercise. Spine (Phila Pa 1976) 2004; 29:2350-2356
4. Deare JC, Zheng Z, Xue CC, et al Acupuncture for treating fibromyalgia. Cochrane Database Syst Rev; 2013;5:CD007070.
5. Fogleman C. The Evidence for Acupuncture in Cancer Therapy. J Lanc Gen Hosp. 2012; 7 (3):78=83.
6. Janna L. Friedly, MD et al A Randomized Trial of Epidural Glucocorticoid Injections for Spinal Stenosis. N Engl J Med 2014; 371:11-21;July 3, 2014
7. Manchikanti L. et al. Effectiveness of therapeutic lumbar transforaminal epidural steroid injections in managing lumbar spinal pain. Pain Physician. 2012 May-Jun;15(3):E199-245
8. Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150:971–979
9. Nissen SE, Yeomans ND, Solomon DH et al. for the PRECISION Trial Investigators. Cardiovascular Safety of Celecoxib, Naproxen, or Ibuprofen for Arthritis. N Eng J Med. November 13, 2016DOI: 10.1056/NEJMoa1611593 (presented at the 2016 Annual Meeting of the Am. Ht. Assoc.)